Side effect of climate change, the consumption of our earth’s resources, as well as the side effects of intensive livestock farming, is that attention is turning to a ‘holistic consciousness’. Let us hope for time. Thinking in (larger) contexts instead of treating symptoms, which is why we constantly problems to the future. How much longer? A new way of thinking is needed, which could be called ecological or systemic thinking, and which goes hand in hand with a different appreciation of nature and life: in search for integrity (Verhoog et al., 2003).
In late 2024, Hanna Mayerhofer and Isabel Pali-Schöll published an article entitled: One health, the influence of environment, detergents and hygiene on barrier, microbiome and allergy. The article comes from the group of scientists working on allergy, asthma, raw milk, and barn environment in Austria. The ‘cow barn pill’ based on the whey protein beta-lactoglobulin was developed by their colleagues. Now the focus is on ‘one health’ from their expert perspective on immunology.
Our mucous membranes built the contact to world outside
As organisms, we have contact with the outside world through our skin and especially the mucous membrane. We know the mucous membrane in the nose, mouth and further intestinal tract, as well as the vagina. The mucous membrane borders us and provides the immunological communication between outside world and our inner world. Thereby, you still must think of the inside lumen of your intestine as (a relative) outside world, and only by passage through the intestinal wall, substances (as digested food) encounter our real inner world, our blood and lymphatic tubes.
The authors introduce a fictional person, the farmer’s wife Gisela, and assess her daily actions and choices, how they affect mucosal and immunological health status. Our lifestyle, the choices of how we and what we eat, whether we have pets, how we deal with infections and antibiotics, how we wash and brush our teeth, how we move influence our microbiome, the composition of the mucous membrane, the gut. Our daily choices disrupt or heal the barrier functions of all that mucous tissue. Using a series of examples from the ordinary life of this fictional farmer’s wife, the authors ask for awareness, how our lifestyle affects our immunological health. Gisela is a farmer’s wife, who has cows of her own. Like any other human being, she washes herself, brushes her teeth, washes her clothes, snacks between meals and eats full meals. Of course, Gisela drinks her own raw milk. She walks her dog and is in contact with all kinds of other animals on the farm. She is stressed, takes antacids and occasionally a sleep aid
How is our immunity affected?
What we donot realise is how industry uses numerous excipients to ‘improve’ products such as soaps, detergents and skin creams. For instance, surfactants are added to soaps, detergents and toothpaste (Sodium sulphates). Why? Because of foaming, (de-)emulsifying or plaque removal. Such substances denature proteins, but therefore also affect the development of allergic inflammation. Even though we rinse our mouths well after brushing and a washing machine removes soap residues, residues of these substances encounter our skin and mucous membrane. Enzymes and perfumes are added, which influence the functioning of barrier functions. For instance, dishwasher detergents contain alcohol ethoxylates, toxic surfactants, which stick to the shiny dishes, and we ingest daily. These substances also adversely affect the barrier function of the mucous membrane, give rise to a form of dysbiosis and provide space for pathogens such as Staphylococcus aureus to gain a foothold in the gut microbiome.
The idea, that you ‘must’ shower daily to be clean and fresh, has crept into our society. Increased personal hygiene due to the Covid crisis, among others, also leads to frequent hand disinfection. The frequent use of antimicrobial disinfectants is giving rise to resistance of ‘common bacteria’. However, increase in asthma among nurses is associated with the frequent use of disinfectants such as triclosan.
There is also frequent and easy use of antibiotics, both human and livestock (also used as growth promoters). It leads not only to ineffective drugs, but also to an increase in asthma and allergy sensitivity, probably again because the gut microbiome changes. In particular, the (repeated) use of antibiotics at a young age leads to immunological problems later, that become visible as hypersensitivity and asthma. Finally, the use of medications such as antacids and anti-psychotic drugs, also negatively affect the gut composition. The authors thus call attention to chemical-synthetic substances, made by industry to improve products, to make their use easier or only to look better and more attractive. We are overloaded with these additives in our convenience and appearance-oriented society. Further, part of the one-health concept is the avoidance of symptom-fighting measures. Indeed, from that, a downward spiral in terms of health ensues when you don’t move beyond symptom-focused solutions.
One health and food choices
Of course, the diet, the foods we consume daily play an important role in the development of the gut microbiome. Dietary fibre acts as a prebiotic, and certain sugars promote the diversity of the microbiome. A well-functioning gut, which does not ‘leak’ large molecules through the intestinal wall, is crucial for our immunity. Besides food as a prebiotic, the authors name the potential probiotic effect of fermented foods, such as sauerkraut and other fermented vegetables, kombucha, yoghurt, kefir, miso, tempeh or kimchi. Remarkable outcome is, that the probiotic bacteria in such fermented foods have rather an indirect effect on the microbiome. They do not multiply themselves in the gut but change the remaining microbiome via their metabolic products. Among other things, they are known to increase butyrate (butyric acid) in a healthy gut.
What has been often investigated is the impact of the fatty acid composition of our diet. There are numerous fatty acids, which by themselves (concentration) or through their ratio to others (omega-6/omega-3 ratio) influence the gut microbiome. The so-called Mediterranean diet is in the spotlight for its anti-inflammatory properties. Looking at milk fat, dairy (regardless of heating) can contribute to the balance between n6 and n3, especially by eating milk products from grazing cows, which are not or hardly supplemented with maize silage and concentrates. There is now and array of milk fatty acids, including the ‘pasture’ CLA (C18:2c9t11) and its precursors trans-vacetic acid (C18:1t11) and trans-palmitoleic acid (C16:1t9), which are associated with positive health, especially when it comes to cardiovascular disease and type2 diabetes.
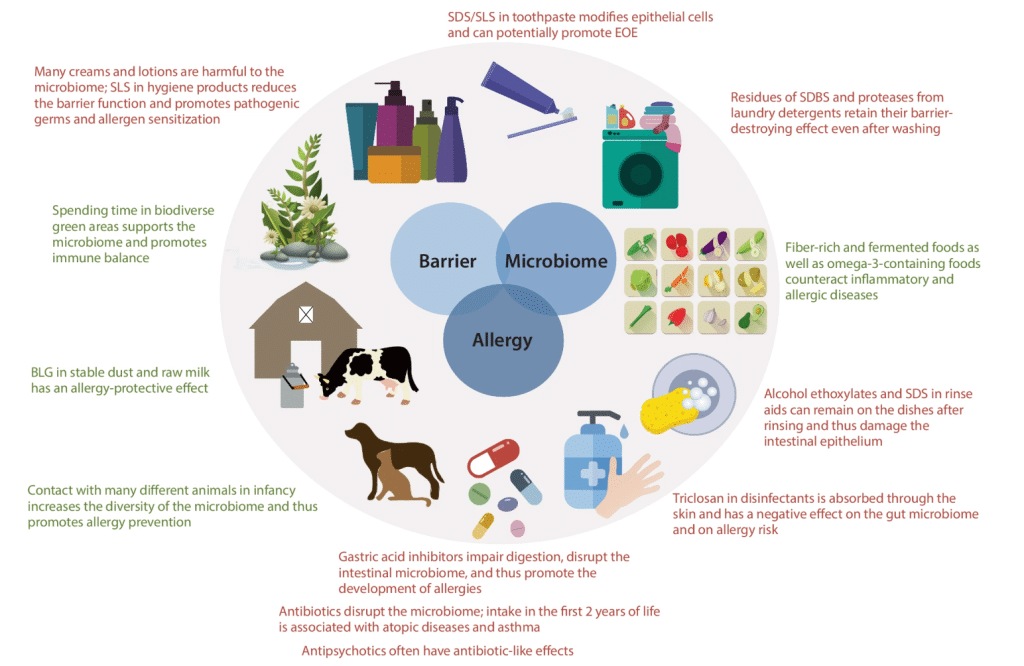
Summary of how daily choices affect immunity (as allergy, via barrier functions and the microbiome) negatively (in red) or positively (in green). (copied from Mayerhofer and Pali-Scholl article, 2024)
Conclusion one-health
In conclusion, the authors state, we encounter numerous factors in our daily lives, which can affect the human microbiome – from nose to gut to skin – and the barrier of our skin and mucous membranes, mostly negatively, but also prositively.
The microbiome has an impact on asthma and allergies. The one-health approach focuses on the avoidance of numerous new, lab-made substances that we have incorporated into our lives. Many of them are excipients (foam firming, high gloss, emulsifying, …) that ‘improve’ simple, often age-old processes. It turns out that many of these substances alone or together affect our microbiome. When we reconnect with home remedies from mother’s and grandmother’s time, we avoid many of these negative effects of modern chemistry. The same goes for choices in nutrition. There is more and more information, how you can boost the microbiome through foods.
As for milk products, fermented products are of great importance due to their pre-, pro- and post-biotic effects. Also direct contact with animals, cows, the barn and consumption of raw milk play a crucial role in the composition of the microbiome, proper barrier functions resulting in a reduction of asthma and allergies in our western society.
Literature
- Mayerhofer, H., & Pali-Schöll, I. (2024). One health: the impact of environment, detergents and hygiene on barrier, microbiome and allergy. Allergo Journal International, 1-11. Download here.
- Verhoog, H., Matze, M., Van Bueren, E. L., & Baars, T. (2003). The role of the concept of the natural (naturalness) in organic farming. Journal of agricultural and environmental ethics, 16, 29-49.




