Take home message
- Three recent studies suggest a positive effect on the intestinal flora from raw milk compared to pasteurised milk. This is found, among other things, in the volatile fatty acids that are formed in the intestine and the colonisation of bacteria found in raw milk in the gut.
Adults in the US and the consumption of raw milk/ raw milk dairy
In the first study (Baars et al., 2019), 327 American consumers were asked about the effects of a diet switch from pasteurised milk products to raw milk products. After switching, the consumption of milk (now as raw milk) almost doubled, while the consumption of cheese decreased slightly.
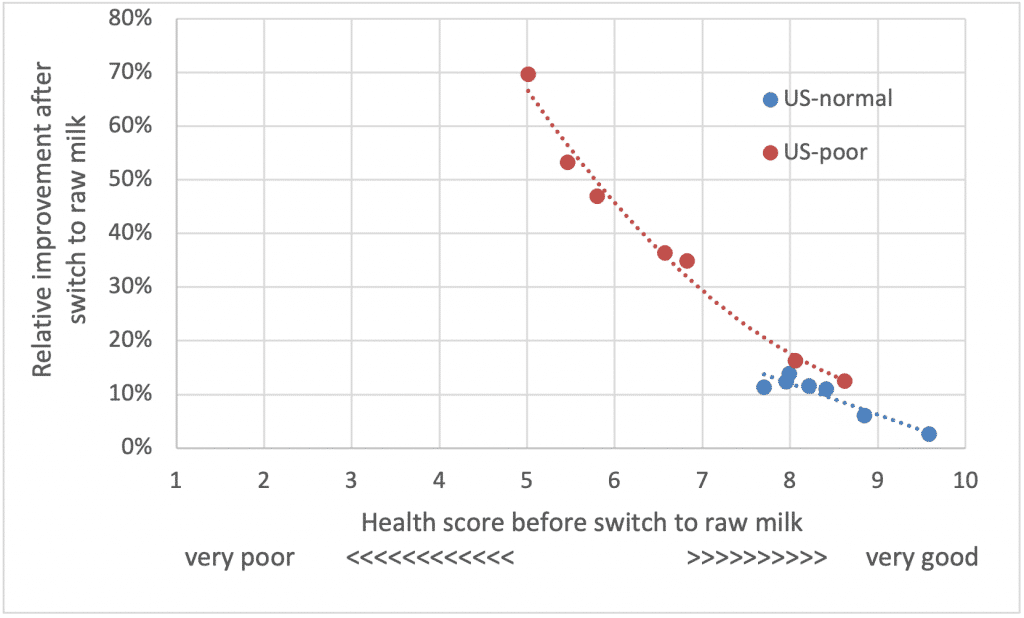
Participants scored their health, immunity, their mood, their intestinal and skin complaints before and after switching to raw milk dairy. The group was divided into people without chronic problems (normal health; n=171) and people with chronic problems (poor health; n=156), (Figure 1). This distinction was important, because these results had one of the largest impacts on the outcome scores.
The score for each participant was calculated both before after switching to raw milk dairy on a scale of 1 (“very bad”) to 10 (“very good”). Those with a low health score beforehand demonstrated a stronger percentage improvement compared to those who started with a higher score. The improvement in the ‘poor’ group was between 12% and 70%, while this is in a much smaller range in the ‘normal’ group (2%-13%).
It is important to note that those who suffered from chronic problems had the highest raw milk consumption, although drinking of raw milk is not advised by food authorities for those with a weakened immunity.
The intestinal flora of Irish students and raw milk
A remarkable study was published in 2020, in which 24 participants on a residential organic farming and nutrition training course were fed almost entirely with products from the farm, including raw milk from Jersey cows (Butler et al., 2020). Questionnaires determined participants’ mood, anxiety, sleep, and physical movement, as well as quantities of foods eaten both before and during the course. At the start and during the last week of the course, faecal samples were collected, which were analysed with DNA techniques for the composition of the intestinal flora and for short-chain fatty acids.
Table 1. Change in the intake of nutrients and foods. The increase or decrease is indicated as the ‘% change’ and only those items are included that have at least a tendency for significance (P<0.10).
| Nutrients | Prior course | Post course | % change | Sign. |
| Fat (g) | 94 | 128 | 36% | ~ |
| Saturated fatty acids (g) | 34 | 49 | 44% | * |
| Vitamin A (mu g) | 715 | 1505 | 110% | * |
| Vitamin B12 (mu g) | 7.8 | 11.0 | 41% | ~ |
| Vitamin D (mu g) | 3.6 | 5.1 | 42% | ~ |
| Food items | ||||
| Red meat | 0.62 | 0.85 | 37% | ~ |
| Organ meat | 0.04 | 0.11 | 175% | * |
| Fish | 0.55 | 0.68 | 24% | * |
| Fried food | 0.21 | 0.30 | 43% | * |
| Potato | 0.34 | 0.49 | 44% | ~ |
| Full fat milk products | 2.03 | 3.59 | 77% | ~ |
| Skimmed milk products | 0.21 | 0.36 | 71% | * |
| Processed meat | 0.58 | 0.33 | -43% | ~ |
| Fruit | 2.02 | 1.38 | -32% | * |
| Vegetables | 0.30 | 0.22 | -27% | ~ |
| Intake milk products per day | ||||
| Full fat milk products (portion) | 2.03 | 3.59 | 77% | ~ |
| Skimmed milk products (portion) | 0.21 | 0.36 | 71% | * |
| Total milk products (portion) | 2.24 | 3.35 | 50% | ~ |
| Raw milk (mL) | 23 | 239 | 939% | *** |
| Raw milk products (portion) | 0.01 | 1.20 | 11900% | *** |
The shift in food can be characterised as follows: more fat was eaten, especially from animal products (dairy, red meat) and less processed meat, vegetables and fruit. Most striking is the change in milk products and in particular the amount of raw milk consumed, which was very low prior to the course. The intake of several important vitamins increased from the switch in diet.
The DNA analysis of the intestinal flora shows a highly significant change in the genus Lactobacillus, which was found in all students. Leuconostoc and Enterococcus did not change, while the psychotrophic bacteria Pseudomonas and Acinetobacter were not found. These results show that some bacteria can probably reach the gut, others are digested before reaching the gut. Furthermore, the researchers found a significant correlation between raw milk intake and the increase in quantity of Lactobacilli, which also correlated with total dairy products, a strong indication that raw milk products have influenced the intestinal flora. The differences in intestinal Lactobacillus concentration could not be further correlated with the measured sleep, anxiety, stress and activity parameters. However, when the participants were divided into two groups based on the score of stress or depression at the start, those that scored highly showed a decrease in stress and depression over the 12-week period.
Finally, changes were found in the short-chain fatty acids in the participants’ faeces after 12 weeks of diet. The strongest increase was in Valeric acid and to a slightly lesser extent with Propionic acid, both odd chain fatty acids. These short-chain fatty acids are metabolic products of the intestinal flora and the increase in Lactobacilli in the intestine may be responsible for this.
The increase in Lactobacilli could be due either to the increased absorption of Lactobacilli from the milk or to better growth of these bacteria within the gut on the sugars present in the milk. This suggests that raw milk either acts as a probiotic or as a prebiotic food.
The intestinal flora of mice
Utrecht mice were fed different types of milk at a young age: raw full fat, raw skimmed (0% fat) and pasteurised full fat (Abbring et al., 2021). The mice were sensitised for allergy (tolerance model of food allergy) and at the end of the study all animals were triggered with Ovalbumin (chicken protein) to measure their sensitivity to an unknown protein. The mice fed full-fat pasteurised milk responded with an allergic reaction, whereas those fed raw full-fat and semi-skimmed raw milk showed no reaction. This indicates that the allergy sensitivity is caused by the heat-sensitive whey proteins and not the milk fat. Mouse droppings were collected at various intervals during the trial and analysed.
Before the test groups were formed, the gut microbiomes of the mice were identical. After more than 30 days of treatment, there were differences between the groups in nine microbial groups. Several bacterial groups increased after consumption of raw milk and there was a correlation with the production of another short chain fatty acid, butyric acid, in the large intestine. Differences were already visible after 8 days of milk consumption but were more pronounced in the measurements on later days, suggesting that these bacteria need time to colonise the gut. Overall, there is a shift towards more pro-inflammatory bacteria and a decrease in anti-inflammatory bacteria in the intestines of mice fed with pasteurised milk, suggesting that the type of milk consumed affects inflammation pattern in the gut.
Reflections on these studies
The switch in diet in the Irish study led to an increased colonisation of the gut with Lactobacilli, finding a correlation with raw milk and raw milk dairy consumption. The study indicates a probiotic or prebiotic effect from raw milk.
The American study also points to benefits from raw milk, but it should be noted that consumers also consumed small amounts of raw milk kefir and raw milk cheeses. Some raw milk as it is consumed in the US, is rather low in bacteria as producers strive for low bacterial counts in the milk (Berge et al., 2020). However, raw-milk kefir and other fermented dairy may produce a benefit from the inoculation of starter cultures creates an acidic dairy product high in Lactobacilli and yeasts.
Consumers of raw milk kefir often notice a relapse of their complaints, if they stop drinking kefir. This may indicate that a regular consumption of such probiotic bacteria is necessary to maintain the changes in the adult gut. The intestine can become “empty” again if consumption does not resume quickly.
It is noteworthy that the shift in the Irish diet is not in line with current advice for a healthy diet (more fruits, vegetables, less saturated fat). This outcome can be compared with the farmers in the Swiss Lötschendal, who were visited by Weston Price in 1930 and 1931. Swiss farmers and their children had a similar diet to the Irish students, but perhaps departing even further from standard advice, with low intake of fruit and vegetables and high intake of fermented products such as sourdough bread, raw milk and raw alpine cheese. These farmers and their children must have ingested enormous amounts of bacteria from their foods and were observed to be very healthy with a very normal to good life expectancy for that time.
Conclusion
Raw milk, either full fat or skimmed, influences the composition of the intestinal flora in humans and does not produce the allergic reaction in mice that pasteurised milk does. Lactobacilli colonised the gut in adults consuming raw milk and dairy products. It remains unclear what the relationship is between changed gut flora and the outcomes in mood and health. Clinical research with defined patient groups is therefore necessary.
References
- Abbring, S., Engen, P. A., Naqib, A., Green, S. J., Garssen, J., Keshavarzian, A., & van Esch, B. C. (2021). Raw Milk-Induced Protection against Food Allergic Symptoms in Mice Is Accompanied by Shifts in Microbial Community Structure. International journal of molecular sciences, 22(7), 3417.
- Baars, T., Berge, A. C., Garssen, J., & Verster, J. C. (2019a). Effect of raw milk consumption on perceived health, mood and immune functioning among US adults with a poor and normal health: A retrospective questionnaire based study. Complementary Therapies in Medicine, 47, 102196.
- Baars, T., Berge, C., Garssen, J., & Verster, J. (2019b). The impact of raw fermented milk products on perceived health and mood among Dutch adults. Nutrition & Food Science.
- Berge, A. C., & Baars, T. (2020). Raw milk producers with high levels of hygiene and safety. Epidemiology & Infection, 148.
- Butler, M. I., Bastiaanssen, T. F., Long-Smith, C., Berding, K., Morkl, S., Cusack, A. M., … & Dinan, T. G. (2020). Recipe for a healthy gut: intake of unpasteurised milk is associated with increased lactobacillus abundance in the human gut microbiome. Nutrients, 12(5), 1468.




